Liver cirrhosis
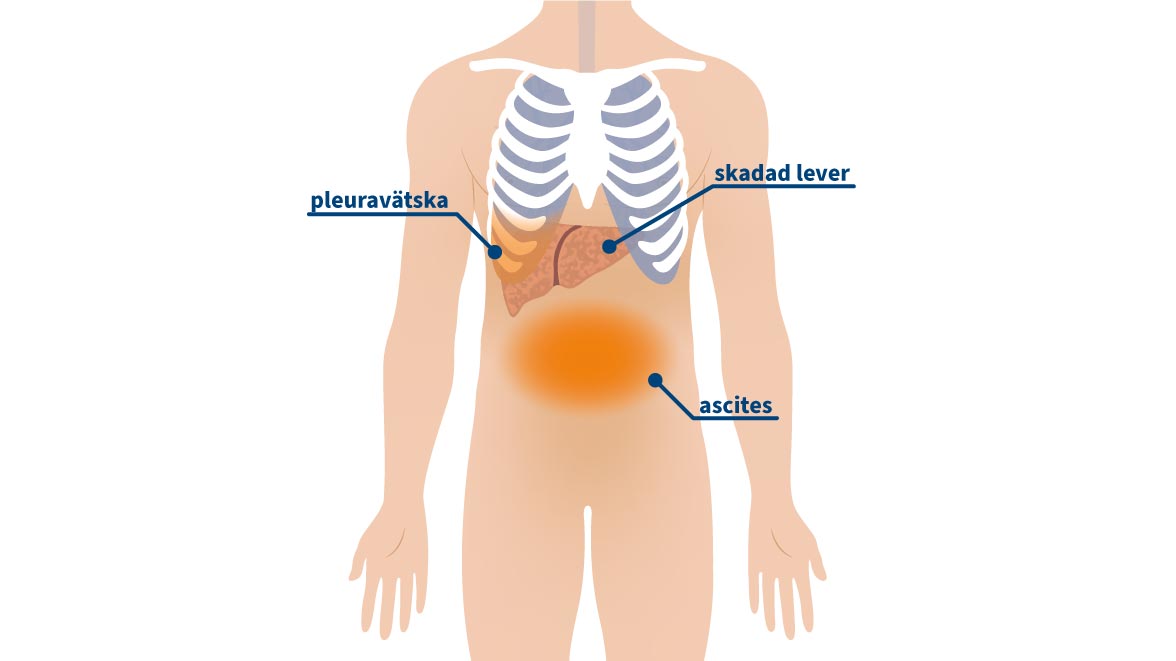
Do you or a loved one suffer from cirrhosis of the liver and have developed ascites (fluid in the abdomen) or pleural effusion (fluid in the lungs) as a result of the disease? What can you do to alleviate these troublesome symptoms?
We have the solution!
In 60% of patients with liver cirrhosis, ascites (abdominal fluid)1 develops during the course of the disease. More rarely, pleural fluid (water in the pleura) develops. In addition to the disease itself, this accumulation of fluid in the abdomen or chest is a major burden for the patient. Symptoms include pressure or pain in the stomach or chest, digestive problems, nausea, increased abdominal girth, shortness of breath or unsteady gait.
To alleviate these symptoms, there are different treatment options that the doctor can choose from:
- Repeated one-time tapping
- TIPS (for ascites)
- Pleurodesis (sticking together of the pleural sheets)
- Indwelling drainage catheter for home drainage

What are the benefits of the ewimed drainage kit?
- Independent, fast and safe drainage at home
- No further hospital stays for dehydration
- Ease of use and patient safety
- No repeated, painful one-time tapping
- A single procedure with local anesthesia to insert the catheter
- Highest safety thanks to the unique connection between the catheter and the drainage set
- Increased independence and mobility for you as a patient
- Reduced risk of infection
- All patients in one study would choose the indwelling catheter again2
Patients and families talk about liver cirrhosis...

Hello, my name is Brigitte. I was infected 10 years ago with the hepatitis C virus. I don’t understand how it could happen. Since then, I have tried different treatments and therapies, but none of them have made me well. Nowadays, I have mostly accepted that I will not recover. Due to the chronic inflammation, cirrhosis of the liver has developed, which causes me to have frequent ascites. My doctor has implanted a catheter to drain the fluid. If necessary, I can connect it to a container and drain the fluid myself. It’s really great, as it saves me a lot of hospitalization.
- Brigitte, 38 years old, hepatitis -

To relax from the stress of everyday life, I liked to drink a little in the evening. But it’s paying off now: the years of steady alcohol consumption have really damaged my liver. When the first signs of liver disease appeared, I ignored them, or told myself it was just something harmless that would soon go away. But eventually I started having real pains in my stomach and shortness of breath. I couldn’t take it anymore and my wife took me to the emergency room. There, after some tests, the doctors diagnosed advanced cirrhosis of the liver – what a terrible news! The doctors drew up a treatment plan, which I am also sticking to. Most of the symptoms are now under control. But the worst thing was that I got fluid in my stomach again, which caused these severe pains in my stomach and shortness of breath. So the doctors suggested putting in an indwelling catheter – well, it’s worth a try. And lo and behold: when fluid forms in my stomach again, I can drain it myself at home. Without any outside help. Since then, I haven’t had any stomach pain or shortness of breath either.
My liver will not recover, but by sticking to the treatment plan the doctors gave me and not drinking a drop of alcohol anymore, I can at least keep the cirrhosis from progressing further.
- Sven, 53 years old, alcohol-induced liver cirrhosis

My wife has been drinking a lot of alcohol every day for many years. She always thought I didn’t notice, has tried to keep it a secret and has always denied that she is an alcoholic. But eventually I got her to agree to detox. We all thought she had made it, but then she started drinking on the sly again.
Three months ago, within a couple of days, she got a really big belly, as if she was pregnant. She was having trouble breathing and was in pain, I could see it in her face. She refused to go to hospital at first, but fortunately she was eventually persuaded. She was admitted and diagnosed with type B cirrhosis of the liver, with a type C tendency. The doctors drained the fluid in her stomach and she felt a little better. After a few days she was allowed to go home. But the fluid in her stomach came back and had to be drained again. The doctor suggested that we implant a catheter. But even there she refused and absolutely did not want it. After four weeks and three more one-time drains, she let them put in a drainage catheter. Now we can drain the fluid ourselves at home, so she doesn’t have much pain anymore and she doesn’t have shortness of breath. Since then, she is generally feeling better. I am really happy about that.
- Bernd, 56, family member of patient with alcohol-induced liver cirrhosis -
ewimed service
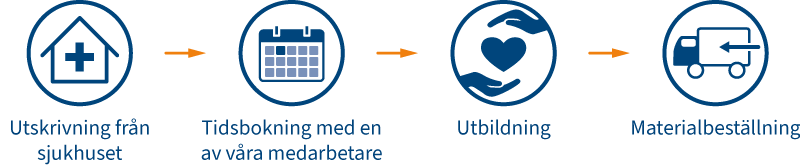
The catheter used to drain the fluid is a soft, pliable silicone tube. The implantation is a small, minimally invasive procedure with a short hospital stay. When you are discharged from hospital, one of our staff will book a training session. During the training, we will explain to you or your healthcare professional step-by-step how to use our drainage kits and help you find out how best to order more material.
Indwelling drainage catheter explained in 2 minutes
You are currently viewing a placeholder content from YouTube. To access the actual content, click the button below. Please note that doing so will share data with third-party providers.
More InformationMore information about cirrhosis of the liver
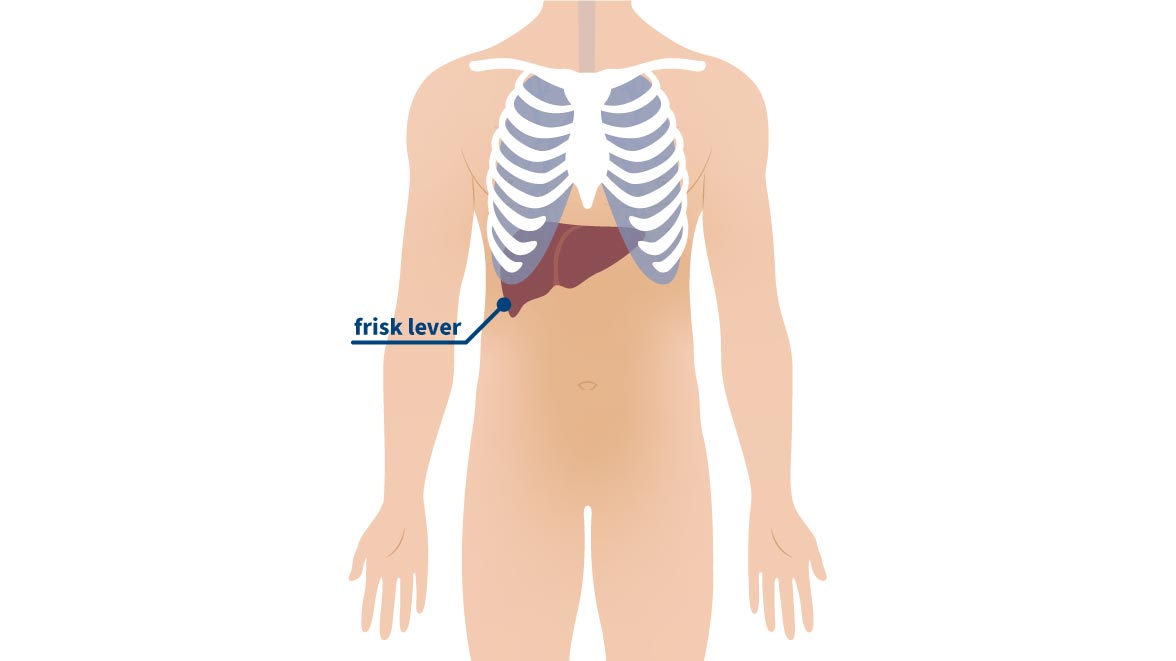
Among other things, the liver breaks down toxins that have entered the body. If the liver is diseased or damaged, it can no longer function properly and cannot break down all the toxins in our body. In advanced stages, this is known as cirrhosis of the liver.
Cirrhosis of the liver is an advanced stage of liver disease, when liver cells are damaged and replaced by scar tissue (fibrosis). This tissue cannot maintain the function of healthy liver tissue.
In liver fibrosis, also known as hepatitis, the liver tissue is replaced by connective tissue. The structure of the liver remains. If the cause can be treated, the liver tissue can recover. If the cause is not treated, this can lead to cirrhosis, which is permanent damage to the liver.
Cirrhosis comes from the Greek word kirrhós, meaning ‘yellow’. Because of the scarred tissue, the liver often turns yellowish.
The most common cause of liver cirrhosis is alcohol abuse, but other diseases can also lead to liver cirrhosis, such as chronic or autoimmune liver diseases, fatty liver, rare metabolic diseases, but also hepatitis viruses (most commonly hepatitis B or C).
To prevent liver cirrhosis from progressing, the underlying disease must first be treated.
Cirrhosis of the liver is often detected very late, when there are no obvious symptoms at first. It can be diagnosed by changes in blood counts, imaging (such as an ultrasound scan or an MRI (magnetic resonance imaging)) and a liver biopsy (a sample of liver tissue).
At a later stage, cirrhosis of the liver can lead to a feeling of pressure in the upper abdomen, flushing, nausea or skin changes. Some examples of skin changes are:
- spider veins (star-shaped vascular changes), especially in the face and décolleté
- Itching
- Hair loss on the stomach
- Redness in the palm of the hand
- White nails
Other signs can be:
- Jaundice (skin and eye whites turn yellow)
- Ascites (fluid in the abdomen), which in turn causes abdominal pain and shortness of breath. It can also lead to peritoneal infection and kidney failure.
- Increased blood pressure in the portal vein (because the liver is damaged, blood flow is disturbed and blood collects in front of the liver. This leads to increased pressure in the portal vein).
- Weight loss
- disruption of brain function (because the liver is damaged and cannot break down all the toxins, it can damage the brain)
- Liver cancer
The progression of liver cirrhosis can be stopped once the cause is known. At an advanced stage, a liver transplant is possible.
If ascites (abdominal fluid) or pleural fluid (fluid in the pleura) develops, this should be treated to avoid further problems. In case of recurrent fluid, a drainage catheter can be implanted. A drainage set can be attached to the catheter as prescribed by the doctor to drain the fluid. This can easily be done in the patient’s home.
Do you have any questions?
Contact us now or click here to find a selection of frequently asked questions.
1MinT, et al: Management of refractory ascites in patients with cirrhosis. British Society of Gastroenterology. 2019
2Selvanet al: Case Report: Indwelling Pleural Catheter Based Management of Refractory Hepatic Hydrothorax as a Bridge to Liver Transplantation. Frontiers in Medicine. 2021